What is Transvaginal Mesh?
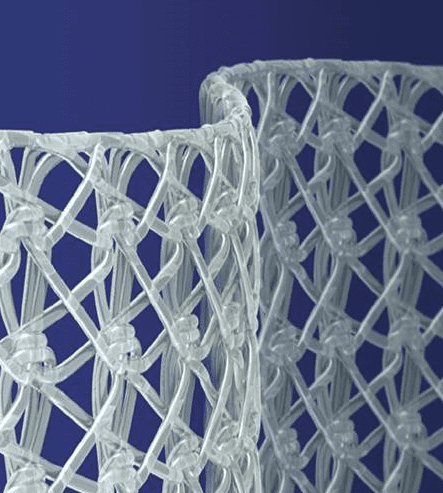
Transvaginal mesh is a medical device implanted to treat stress urinary incontinence (SUI) and pelvic organ prolapse (POP) in women.
Transvaginal mesh is a semi-permeable barrier implanted into a woman as a reinforcing structure to keep her internal organs in place. The device is known as vaginal mesh because it is now typically inserted or placed through the vagina.
Physicians first used what is now referred to as vaginal mesh in the 1950s to treat abdominal hernias. They used the same mesh to treat female stress urinary incontinence and pelvic organ prolapse in the 1970s by cutting it into a different shape.
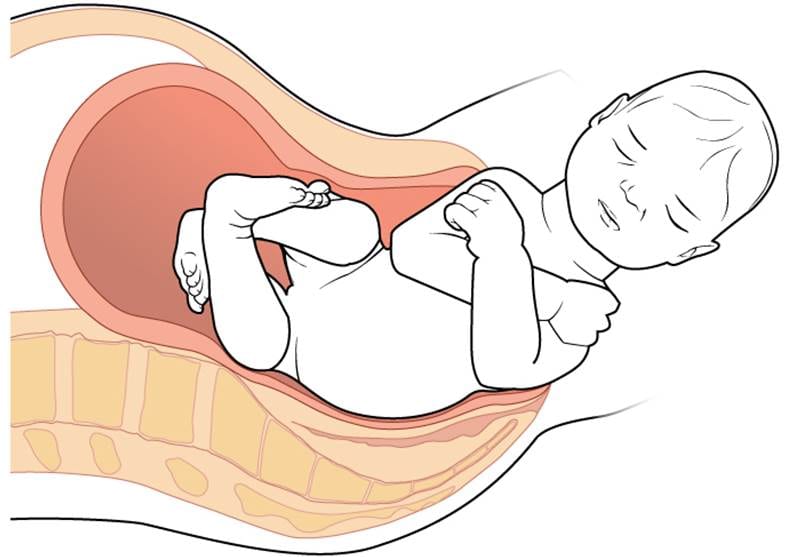
Transvaginal surgical mesh was intended to permanently repair stress urinary incontinence and pelvic organ prolapse. These conditions most often arise in women after hysterectomy, childbirth or menopause. Stress urinary incontinence is the inability to hold urine if physical stress – like bending, lifting, or the stress created by pelvic organ prolapse is experienced. Pelvic organ prolapse occurs when the pelvic muscles of a woman weaken, allowing pelvic organs including the uterus, bladder and rectum to protrude or sag into the vagina.
The term “vaginal mesh” refers to the surgical mesh and mesh products implanted in stress urinary incontinence and pelvic organ prolapse operations. Surgeons use generic mesh they have cut to become suitable for stress urinary incontinence and pelvic organ prolapse repair, or mesh that has been pre-cut by a medical device manufacturer to match the anatomical defects that stress urinary incontinence and pelvic organ prolapse operations should correct.
Stress incontinence is a form of urinary incontinence. Stress urinary incontinence also known as effort incontinence. The condition is due essentially to insufficient strength of the pelvic floor muscles. It results in losing small amounts of urine associated with coughing, laughing, sneezing, exercising or other movements that increase intra-abdominal pressure on the bladder. The urethra is supported by fascia of the pelvic floor. If this support is insufficient, the urethra can move downward causing increased abdominal pressure and allowing urine to pass.
Most stress incontinence in women is caused by the urethra dropping down toward the vagina. Therefore, common surgery for stress incontinence involves repositioning the urethra up to a more normal position. Working through an incision in the vagina or abdomen, the surgeon raises the urethra and secures it with a string attached to bone, ligament or muscle. For severe cases of stress incontinence, the surgeon may secure the urethra with a wide sling. This not only supports the bladder but also compresses the bottom of the bladder and the top of the urethra, further preventing leakage.
Pelvic organ prolapse is a condition in which a woman’s reproductive or pelvic organs fall into or through her vaginal opening. The operations used to correct this condition are called commonly called “sling procedures” because doctors use surgical mesh to create a sling-like structure of support for a patient’s urethra, bladder, or some other organ.
Pelvic organ prolapse can occur when a pelvic organ, such as the bladder or uterus, drops (prolapses) from its normal position in the abdomen into a lower portion of the abdomen and may press on other organs. This happens because the muscles and ligaments holding the pelvic organs weaken or stretch from childbirth, surgery or the progression of menopause. Most women have some type of prolapse, but not all need treatment. Pelvic organ prolapse can also be caused by chronic constipation causing straining, a long-lasting cough, obesity and some types of pelvic organ tumors. Sometimes, the doctor may prescribe exercises, but in other cases, surgery may be advised.
As the use of surgical mesh in stress urinary incontinence and pelvic organ prolapse surgeries increased in popularity in the late 1990s, medical device manufacturers developed and market mesh products in configurations designed specifically to treat these two conditions.
The materials used in transvaginal mesh products on the market fall into the following four categories:
- Non-absorbable synthetic (polypropylene or polyester)
- Absorbable synthetic (poly(lactic-co-glycolic acid) or poly(caprolactone))
- Biologic (a cellular collagen derived from bovine or porcine sources)
- Composite (a combination of any of the previous three categories)
Mesh has also been used for hernias and other disorders requiring surgical support. In the past, most surgical mesh was made of biologic tissues, such as human or bovine connective tissue. Today, transvaginal mesh is most commonly made of a plastic-like substance known as polypropylene coated with biological materials.
Share This